Heroin Overdose Treatment
Discover life-saving heroin overdose treatment solutions. Learn about naloxone, immediate response steps, and long-term consequences.

Heroin Overdose Treatment Overview
Understanding the treatment options for heroin overdose is crucial in saving lives and preventing long-term complications. This section will provide an overview of heroin overdose, emphasizing the importance of prompt treatment.

Understanding Heroin Overdose
Heroin overdose occurs when an individual takes a dose of heroin that exceeds their body's ability to metabolize it safely. The drug depresses the central nervous system, leading to slowed breathing, decreased heart rate, and potentially fatal respiratory depression. Recognizing the signs of overdose is crucial for timely intervention.
Common symptoms of a heroin overdose may include:
- Shallow or absent breathing
- Blue lips or fingertips
- Unresponsiveness or unconsciousness
- Pinpoint pupils
- Slow or weak pulse
If you suspect someone is experiencing a heroin overdose, it is essential to seek immediate medical attention by calling emergency services. Time is of the essence in these situations, and prompt treatment can mean the difference between life and death.
Read about: Empowering Heroin Addiction Facts
Importance of Prompt Treatment
Prompt treatment for a heroin overdose is critical for several reasons. Time-sensitive interventions can prevent severe complications and increase the chances of survival. In 2014, the U.S. Food and Drug Administration (FDA) approved a medication called naloxone (brand name Narcan) to reverse the effects of a heroin overdose. Naloxone can be administered by emergency medical responders, police, family members, caregivers, and others [1].
Naloxone works by binding to the same receptors in the brain that heroin targets, thus blocking its effects. It can rapidly restore normal breathing and reverse the life-threatening consequences of an overdose. Naloxone is available in various forms, including injectable versions and a nasal spray. Its accessibility and ease of administration have made it a vital tool in combating the opioid crisis.
Immediate medical treatment is crucial even if naloxone has been administered successfully. This ensures that the individual receives comprehensive assessment, monitoring, and follow-up care. It also provides an opportunity to address the underlying issues related to the overdose, such as addiction and mental health concerns.
By understanding the signs of a heroin overdose and the importance of prompt treatment, individuals and communities can take proactive steps to address opioid-related emergencies effectively. Educating oneself about overdose prevention, naloxone availability, and emergency response protocols can save lives and contribute to a healthier society.
In the next section, we will explore naloxone as a life-saving medication, including its mechanism of action and administration methods.
Naloxone as a Life-Saving Medication
When it comes to heroin overdose treatment, one of the most critical medications is naloxone. Naloxone is a life-saving medication that can reverse the effects of opioids and prevent fatal consequences. In this section, we will explore the mechanism of action and various administration methods of naloxone.
Mechanism of Action
Naloxone works by binding to the same opioid receptors in the brain that opioids such as heroin attach to. However, naloxone has a stronger affinity for these receptors. By binding to the receptors, naloxone effectively displaces and blocks the opioids, reversing their effects on the central nervous system. This rapid action can restore normal breathing and consciousness, potentially saving someone's life during an opioid overdose.
It's important to note that naloxone has a shorter duration of action compared to many opioids. While opioids may remain in the body for a longer period, naloxone's effects last for only 30 to 90 minutes. This highlights the importance of calling emergency services immediately after administering naloxone, as the individual still requires medical attention. Continuous observation and monitoring of the person's breathing are crucial until emergency care arrives and for an additional 2 hours after the last dose of naloxone is given [2].
Administration Methods
Naloxone can be administered through different methods, depending on the situation and the available resources. The two main administration methods are nasal spray and injection.
Nasal spray: Naloxone is available as a nasal spray, which allows for easy and quick administration. The nasal spray is sprayed into one nostril while the individual lies on their back. The spray delivers naloxone into the nasal passages, where it is absorbed into the bloodstream. This method is particularly useful for individuals who may not feel comfortable or confident administering injections.
Injection: Naloxone can be injected into various sites, including the muscle (intramuscular), under the skin (subcutaneous), or into the veins (intravenous). Injection methods provide rapid delivery of naloxone into the bloodstream, allowing for immediate action. It is crucial to receive training on how and when to use naloxone, read the product instructions, and check the expiration date, regardless of the administration method used [2].
It's important for families with loved ones struggling with opioid addiction to have naloxone readily available. Ensuring that family members and friends are aware of the location of naloxone and how to administer it can be crucial in emergency situations. However, it's important to remember that even after administering naloxone, it is crucial to call 911 immediately for immediate medical attention [2].
In some cases, clinicians may prescribe naloxone alongside prescription opioids to reduce the risk of opioid-related emergency room visits and prescription opioid-involved overdose deaths. The co-prescription of naloxone is recommended by the U.S. Centers for Disease Control and Prevention for certain patients who take opioids [2].
By understanding the mechanism of action and administration methods of naloxone, individuals and their loved ones can be better prepared to respond to opioid-related emergencies and potentially save lives. Access to naloxone, knowledge of its proper use, and prompt action are crucial in combating the devastating consequences of opioid overdose.
Accessing Naloxone and Overdose Prevention
When it comes to addressing heroin overdose, timely intervention is crucial. Naloxone, a life-saving medication, plays a vital role in preventing overdose-related fatalities. In this section, we will explore the availability of naloxone in pharmacies and highlight overdose prevention resources in Canada.
Availability in Pharmacies
In Canada, naloxone is available at pharmacies, making it accessible for individuals in need of overdose prevention measures. This medication can be obtained without a prescription, allowing for prompt access and potentially saving lives. By having naloxone readily available in pharmacies, it becomes easier for individuals, their loved ones, or bystanders to access this life-saving medication when an overdose occurs.
To ensure widespread availability, Health Canada has compiled a list of pharmacies that carry naloxone for overdose prevention purposes. This list enables individuals to locate nearby pharmacies where they can obtain naloxone. By visiting these pharmacies, individuals can acquire naloxone kits and receive instructions on how to administer the medication in case of an opioid overdose. It is essential to familiarize oneself with the process of administering naloxone to effectively respond to an overdose situation.
Managing Opioid-Related Emergency
When faced with an opioid-related emergency, prompt action is vital. It's crucial to know the immediate response steps and follow-up care considerations to effectively manage the situation.
Immediate Response Steps
If you encounter an individual experiencing an opioid overdose, taking immediate action can be life-saving. Here are the steps to follow:
- Call Emergency Services: Dial 911 or your local emergency number immediately to request professional medical assistance. Time is of the essence in treating opioid overdoses, and trained medical professionals can provide the necessary care.
- Administer Naloxone: Naloxone is a medication that rapidly reverses the effects of opioids and can restore normal breathing. If you have access to naloxone, follow the instructions provided with the medication for proper administration. Remember, naloxone works for a limited duration, typically 30 to 90 minutes, while opioids may remain in the body longer [2]. Therefore, it is essential to seek medical attention even after administering naloxone.
- Monitor Breathing: While waiting for emergency medical services to arrive, closely observe the individual's breathing. If their breathing becomes slow or stops, initiate rescue breathing or CPR if you are trained to do so.
- Don't Leave the Person Alone: Stay with the individual until medical help arrives. Offer reassurance and support, as they may be disoriented or frightened.
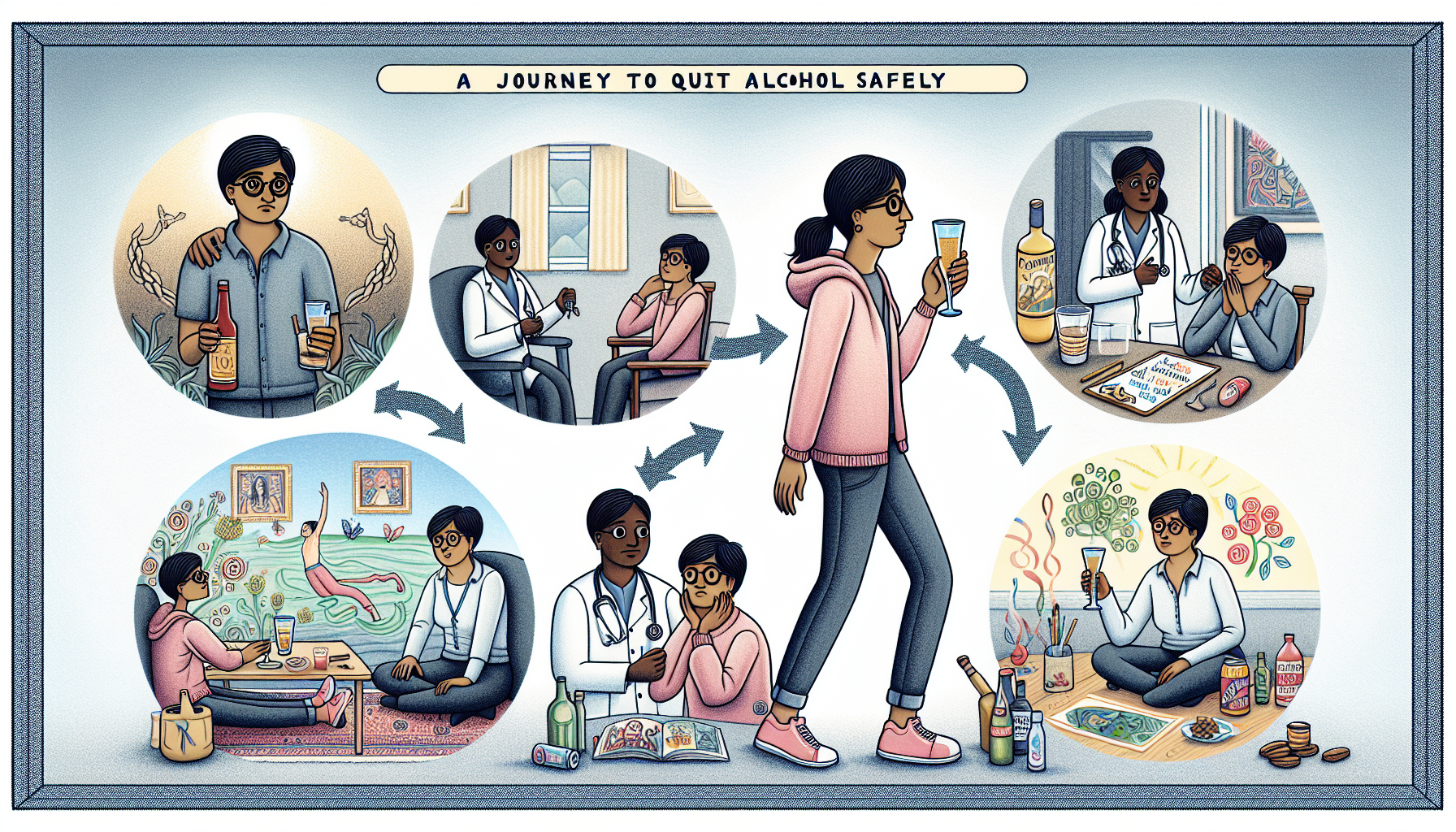
Follow-Up Care Considerations
After the immediate response to an opioid overdose, follow-up care is essential for the well-being of the affected individual. Here are some considerations:
- Seek Medical Attention: Even if the individual appears to have recovered from the overdose, it is crucial to seek medical attention. Opioid overdoses can have long-term consequences and may require further medical evaluation and treatment [1]. A hospital stay may be necessary, especially if there were complications or if there is a history of injecting drugs with needles [1].
- Address Underlying Issues: An opioid overdose can signify a deeper problem with substance use and mental health. It is essential to address these interconnected issues to help prevent future overdoses. Seek support from healthcare professionals, substance abuse counselors, or mental health providers to develop an appropriate treatment plan.
- Education and Prevention: Learning about the risks and dangers of opioid use can help prevent future emergencies. Educate yourself and others about the signs of overdose, the importance of naloxone availability, and safe practices regarding opioid use. By raising awareness, you can contribute to reducing the harm associated with opioids.
Remember, the information provided here is for general guidance, and it is essential to consult healthcare professionals for personalized advice and guidance. Opioid overdoses require immediate medical attention, and timely intervention can save lives. By being prepared and taking the necessary steps, you can play a crucial role in managing opioid-related emergencies effectively.
Complications and Risks
When it comes to heroin overdose, there are significant complications and risks that individuals may face. Understanding the health implications of an overdose and the potential long-term consequences is crucial in addressing this serious issue.
Health Implications of Overdose
Heroin overdose can have severe health implications, primarily due to opioid-induced respiratory depression (OIRD). This is identified as a primary complication and the most dangerous source of adverse health outcomes associated with non-fatal opioid overdose (NFOO) [3]. The respiratory system is severely affected, leading to shallow or slowed breathing, and in some cases, respiratory failure. This lack of oxygen to the body's vital organs can have serious consequences.
Chronic complications associated with non-fatal opioid overdose include:
- Hypoxia-related brain injuries
- Kidney failure
- Heart complications
- Neurologic consequences
- Seizures
- Nerve damage
- Temporary motor paralysis
- Fluid buildup in the lungs
- Stroke and pneumonia from inhaling vomitus [3].
It is important to note that individuals who experience multiple or recurring opioid overdose events are at an increased risk for hypoxic brain damage due to repeated and prolonged hypoxia, leading to white matter damage in the brain [3]. The severity of these health implications can vary depending on factors such as the amount of heroin consumed, the presence of other substances, and the individual's overall health.
Long-Term Consequences
The long-term consequences of a heroin overdose can have a significant impact on an individual's physical and mental well-being. While some individuals may recover with minor health consequences lasting only minutes to hours, such as dizziness, confusion, and ineptness, others may experience more persistent effects [3].
Furthermore, few studies have examined the interplay between pre-existing physical or mental health conditions and subsequent non-fatal opioid overdose. Mental health conditions like depression and suicidality have been strongly associated with opioid use disorder and drug overdose. Addressing these underlying conditions and providing appropriate support is crucial for individuals who have experienced a heroin overdose.
It is important to seek medical attention promptly after a heroin overdose to address the immediate health risks and to ensure proper monitoring and care. If you or someone you know is struggling with heroin addiction, it is essential to reach out to healthcare professionals or addiction support services for assistance. Remember, help and treatment options are available to guide individuals towards recovery and a healthier life.
Addressing Mental Health and Substance Use
When it comes to addressing substance use, including heroin addiction, it is crucial to recognize the interconnectedness between mental health and substance abuse. Individuals struggling with substance use often face underlying mental health conditions that contribute to their addiction. Providing support and resources that address both aspects is essential for effective treatment.
Read about: Startling Substance Abuse Statistics
Interconnectedness and Support
Mental health and substance use are deeply intertwined. Many individuals turn to substances as a way to cope with underlying mental health issues such as depression, anxiety, or trauma. Unfortunately, substance abuse can exacerbate these conditions, creating a vicious cycle. Recognizing and addressing both mental health and substance use is vital for successful recovery.
Support networks play a crucial role in addressing mental health and substance use. These networks can include friends, family, support groups, and mental health professionals. Encouraging open communication and fostering a non-judgmental environment are key to helping individuals feel comfortable seeking help. Providing resources and information on available support networks can empower individuals to take the first step towards recovery.
Resources for Dual Diagnosis
Dual diagnosis refers to individuals who experience both mental health disorders and substance use disorders simultaneously. Treating individuals with dual diagnosis requires an integrated and comprehensive approach that considers both aspects of their condition.
In Canada, there are resources specifically tailored to address the needs of individuals with dual diagnosis. Indigenous peoples, including First Nation, Inuit, and Métis individuals, have access to culturally sensitive resources for substance use treatment, such as the National Native Alcohol and Drug Abuse Program and the National Youth Solvent Abuse Program. These programs aim to provide support that is respectful of cultural backgrounds and addresses the unique challenges faced by Indigenous communities.
Additionally, mental health support is available for individuals struggling with mental health issues related to substance use. This recognizes the complex relationship between mental health and substance abuse. Resources and help are accessible for those in need, emphasizing the importance of addressing both mental health and substance use concerns simultaneously [4].
By recognizing the interconnectedness between mental health and substance use, individuals can access the support and resources they need for recovery. Providing information on available resources for dual diagnosis and promoting understanding and empathy can contribute to a more comprehensive approach to addressing substance use and mental health challenges.
References
Similar articles


















.jpg)

















.jpg)






.jpg)



.jpg)






.jpg)











.jpg)









.jpg)




.avif)



.avif)









